
Overview
The Close Collaboration with Parents training is an educational program for healthcare staff to improve family-centered care in neonatal units including NICUs. In the training, the staff learn about the relationship (communication) with parents and the importance of parents through learning theory, bedside training, and reflections. The family-centered care culture of the neonatal unit will change and improve outcomes for babies and their families after the change in mindset happens with as many staff members.
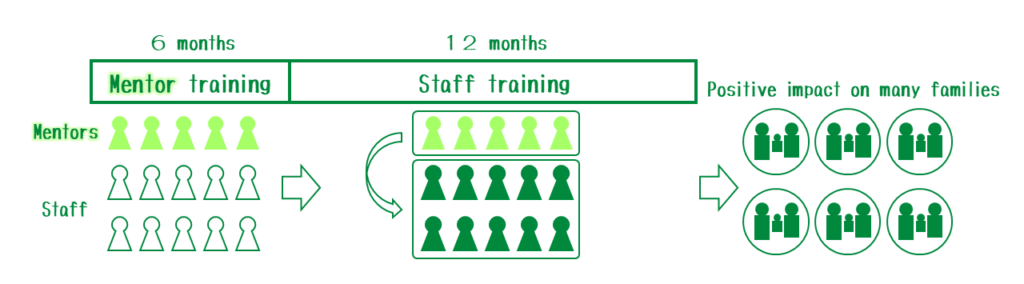
The implementation of the training at the NICU level has two steps. First, mentors (3-4 people per unit in general) implement the training. The mentors, then, mentor the other healthcare staff (mentees). It usually take about half a year for the mentor training and about a year for the healthcare staff training. Thus, it takes about 1.5 years for a NICU to complete the implementation of the Close Collaboration with Parents.
Contents of training
NICUの両親は退院後には、赤ちゃんに関する様々な決定を自分たちで行う必要があり、その準備をNICUで進めるというのは大切なことです。両親がNICUにおける様々な決定に関わることは多くの意味で有益で、これを共同意思決定と呼びます。フェーズIVトレーニングでは、メンティーはEラーニングを通じて共同意思決定に関する理論的背景を学びます。また、医療回診や退院準備の際に共同意思決定をどのように促進するか、そしてその効果について何がわかっているかも学びます。
ベッドサイドでのトレーニングは二つに分けられます。回診のトレーニングでは、両親が医師回診に参加している様子を、可能であれば第三者として観察します。両親が回診の議論にどれだけ参加できているか、またそれを促進または阻害させる要因が何なのかを観察し、振り返ります。また同時に、両親からも話を聞き、より良い回診を行うためのヒントをもらいます。
The training consists of four training phases
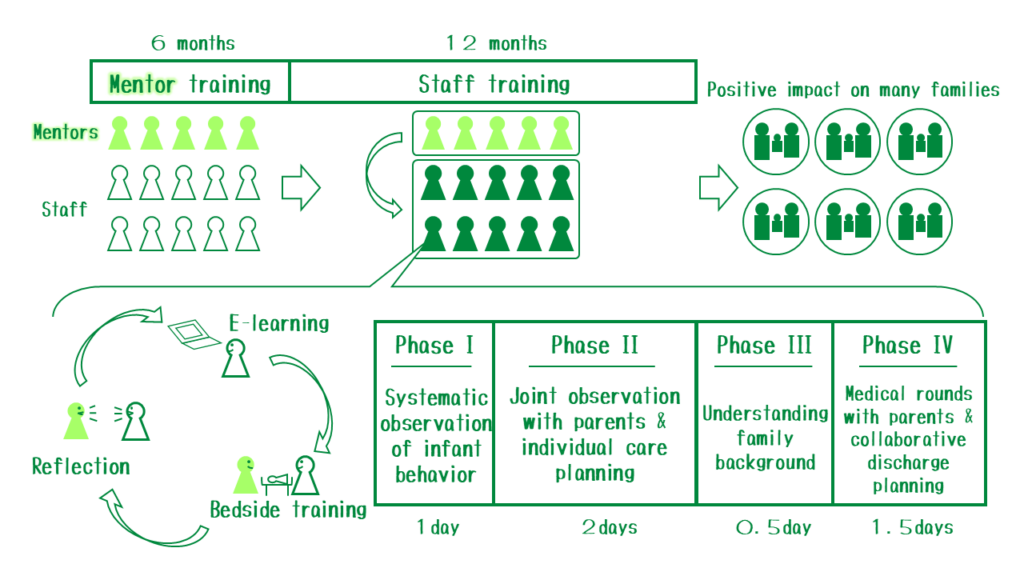
Phase I: Observation of baby behavior
Observation of the baby’s behavior is a prerequisite for individual care and support for the baby according to their developmental stage. This will also serve as the basis of Phase II training onward where we conduct joint observation of the baby’s behavior with the parents. Systematic behavioral observations in the Close Collaboration with Parents training are based on the Neonatal Behavioral Assessment Scale (NBAS), Assessment of Preterm Infant Behavior (APIB), and the Neonatal Network Neurobehavioral Scale (NNNS). Observation includes five levels of baby behavior: physiological signs, muscle tone and motor control, states of alertness, interactive behavior, signs of stress and self-soothing.
In the bedside training, the mentee together with the mentor observes the baby’s behavior and its changes, mainly before, during, and after baby care. In the reflection, they discuss the implications of the observed behaviors and the proposals for better care for the baby.Observation of the baby’s behavior is a prerequisite for individual care and support for the baby according to their developmental stage. This will also serve as the basis for Phase II training, when we conduct joint observation of the baby’s behavior with the parents. Systematic behavioral observations in the Close Collaboration with Parents training are based on the Neonatal Behavioral Assessment Scale (NBAS), the Assessment of Preterm Infant Behavior (APIB), and the Neonatal Network Neurobehavioral Scale (NNNS). Observation includes five levels of baby behavior: physiological signs, muscle tone and motor control, states of alertness, interactive behavior, signs of stress, and self-soothing.
During bedside training, the mentee and mentor observe the baby’s behavior and its changes, mainly before, during, and after care of the baby. Then, in the reflection, they discuss the implications of the observed behaviors and the proposals for the daily care plan of the baby.
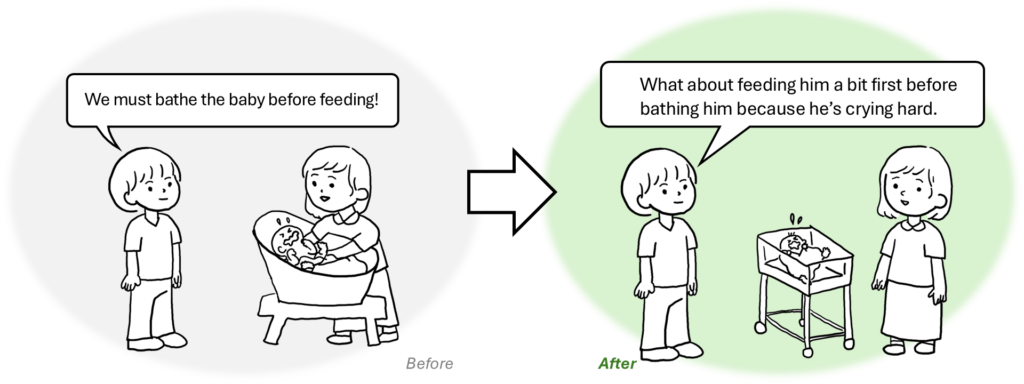
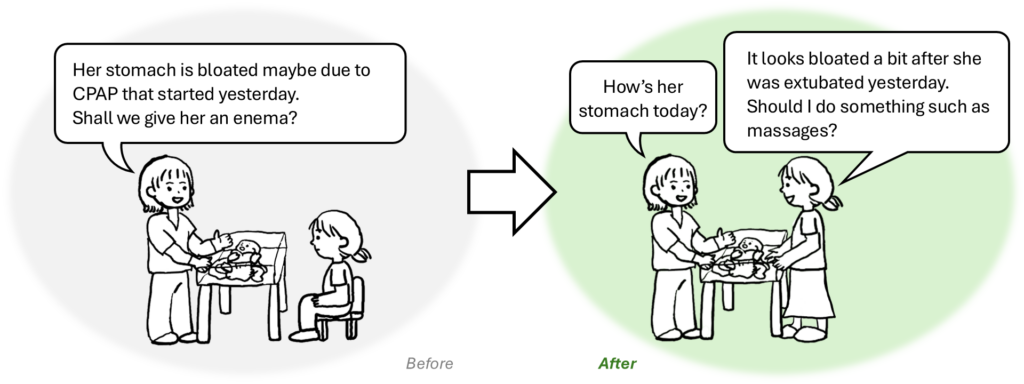
Phase II: Joint observation with parents
Observation of the baby’s behavior is a prerequisite for individual care and support for the baby according to their developmental stage. This will also serve as the basis for Phase II training, when we conduct joint observation of the baby’s behavior with the parents. Systematic behavioral observations in the Close Collaboration with Parents training are based on the Neonatal Behavioral Assessment Scale (NBAS), the Assessment of Preterm Infant Behavior (APIB), and the Neonatal Network Neurobehavioral Scale (NNNS). Observation includes five levels of baby behavior: physiological signs, muscle tone and motor control, states of alertness, interactive behavior, signs of stress, and self-soothing.
During bedside training, the mentee and mentor observe the baby’s behavior and its changes, mainly before, during, and after care of the baby. Then, in the reflection, they discuss the implications of the observed behaviors and the proposals for the daily care plan of the baby.
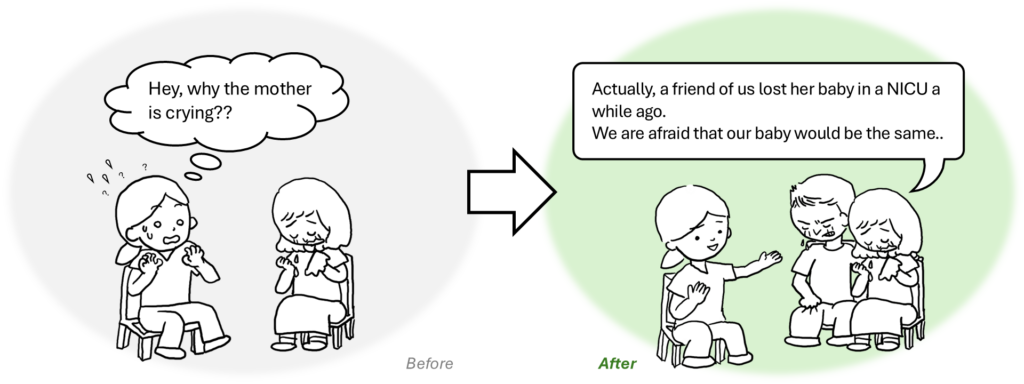
Phase III: Understanding of parents’ background
While Phases I and II focus on the baby, Phase III training allows us to consider the family as a whole. In neonatal medicine, family background and the feelings of family members may not always be considered important. Neonatal health care staff may not know how to apply this information to clinical practice. Phase III training provides an opportunity for parents to go through and share their story of becoming parents for this baby, and allows staff to listen and it and offer better support for the parent-infant relationship.
During bedside training, the mentees and mentor listen to the parents’ story from the beginning of the pregnancy (or even before if necessary) to now. Parents’ storytelling is facilitated by semi-structured questions, namely CLIP-I. In the reflection, mentor and mentee discuss the impact of parents’ experiences on their relationship with the baby and how that can be supported better.
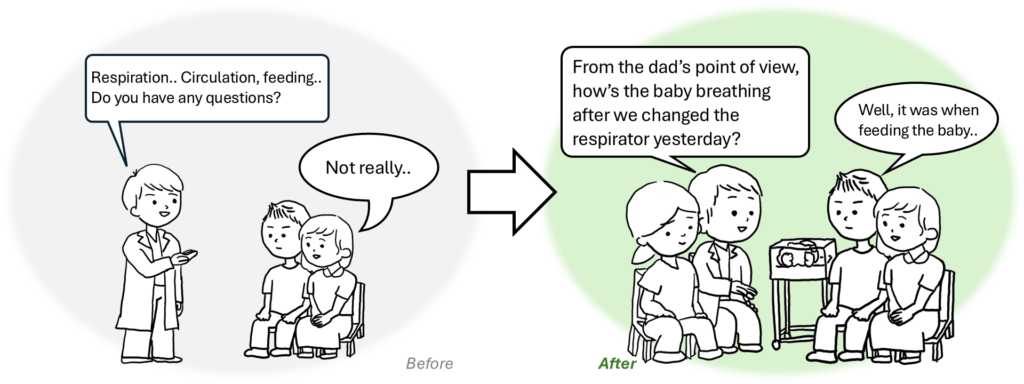
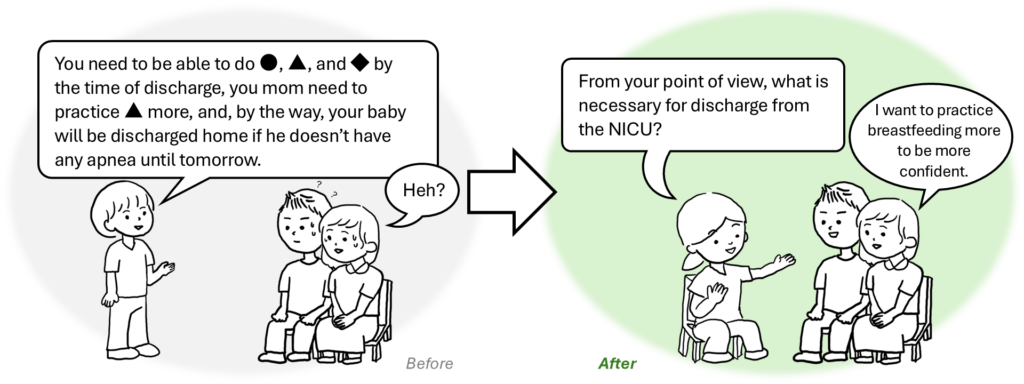
PhaseIV:Collaborative decision-making (parents’ participation in medical rounds and collaborative discharge planning)
Parents need to be prepared for discharge from the NICU because they will be responsible for taking care of the baby and making decisions regarding their baby after discharge. Shared decision-making, parents’ participation in it, is meaningful in many ways. In Phase IV training, the mentee learns the theoretical background of shared decision-making by completing e-learning. They also learn how to promote it during medical rounds and discharge preparation, and what is known about its effects. There are two different types of bedside practices in this phase. One practice focuses on medical rounds. The mentee and the mentor participate in the rounds as a third party, if possible, to observe the staff-parent communication and parents' participation in the round. They observe what promotes and hinders participation. They also interview the parents to understand how to involve parents more in the medical rounds.
The other practice focuses on preparing the family for the transition from hospital to home. A baby’s discharge from the NICU requires not only the baby’s physiological stability, but also the parents who are confident in their ability to care for the baby and are attached to their baby. During reflection, the mentee and the mentor may discuss how early they can start discharge preparation and how they can proceed with it together with the parents.
Implementation process in Japan
We plan to start the training of the Close Collaboration with Parents for the health care staff in Japan. Nagano Children’s Hospital will first complete our implementation process. We will inform you of the details via this web page or any social media.
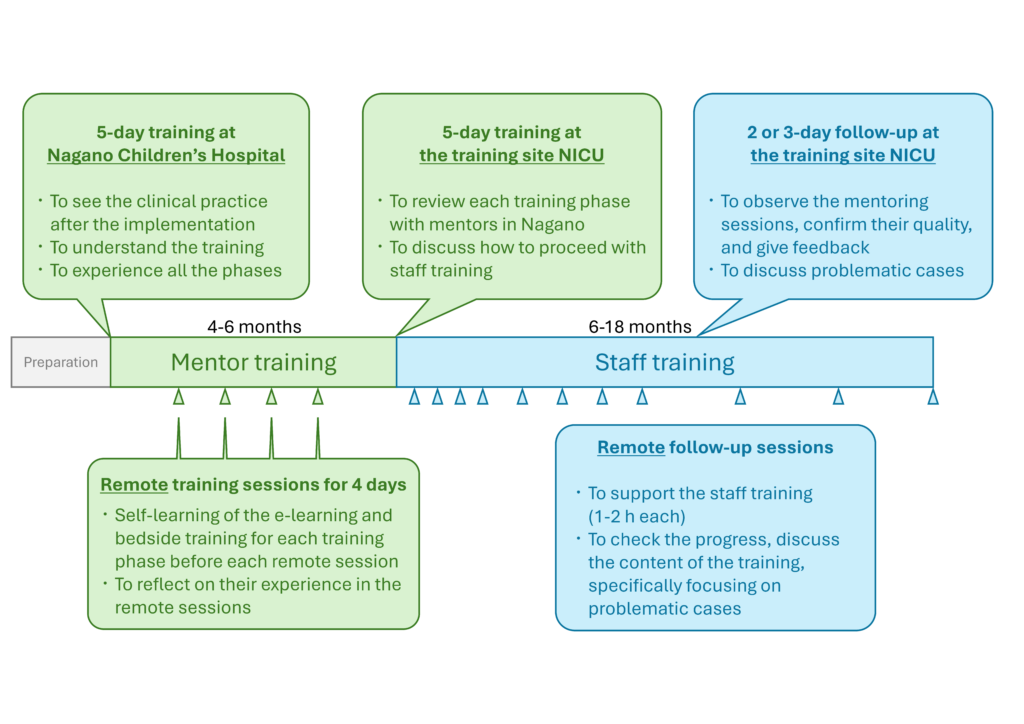
The implementation of the training is NICU-wide in general.
The first step of the implementation is education for local mentors, who receive the training first and train the other NICU staff. Education for local mentors begins with a five-day training at Nagano Children’s Hospital. The local mentors understand the overview of the Close Collaboration with Parents training through the lectures and experiences of each training phase. They can also see how each staff member and the NICU as a whole may change after the implementation. After that, they learn each training phase: learning the theory using the e-learning module, experiencing bedside training, and their experiences being reflected using remote reflective sessions with the training team in Nagano. Education for local mentors is completed after a five-day training in a NICU that implements the training, including the review of each training phase. The local mentors together with the managers of the NICU and the training team in Nagano also discuss the plan of staff training in the NICU. It usually takes about 3 to 4 months for education for local mentors.
Then, the local mentors will start staff training, targeting the other healthcare staff in the NICU. The staff training takes about 14 to 15 months, depending on the number of local mentors and staff and the frequency of the training sessions. Staff training is one of the biggest challenges of the Close Collaboration with Parents. The local mentors need to get used to mentoring and there will be possible inhibitors and unexpected troubles that arise in the course of training. Regular follow-up sessions take place to cope with these problems together with the local mentors, to understand their progress in training, and to encourage the local mentors. The frequency and the duration of the follow-up sessions depend on their individual needs. The training team in Nagano will be responsible for the training of local mentors and other healthcare staff until the staff training is completed. We keep in close contact with the training team in Finland and may provide specific consultation if necessary.
